How Lymphedema Tarda Treatment Is Diagnosed
Introduction
Lymphedema tarda is a rare form of primary lymphedema that typically appears after the age of 35. Because its onset occurs later in life - and because limb swelling can have many possible causes - the process of diagnosing lymphedema tarda is often detailed and systematic. Proper diagnosis is essential not only for confirming the condition but also for guiding the most effective treatment plan. In this article, we explore how healthcare professionals diagnose lymphedema tarda and why each step matters.
Definition
Lymphedema tarda treatment refers to the management strategies used for lymphedema that begins after age 35, focusing on reducing limb swelling, preventing complications, and improving function. Treatment typically includes Complete Decongestive Therapy (manual lymph drainage, compression therapy, exercise, and skin care), along with lifestyle adjustments to support lymph flow. In some cases, pneumatic compression devices, specialized physical therapy, or surgical options may be considered when conservative measures are not sufficient.
Understanding Lymphedema Tarda Before Diagnosis
Lymphedema occurs when the lymphatic system cannot adequately drain lymph fluid, leading to chronic swelling, most commonly in the legs. In lymphedema tarda, individuals are typically born with abnormalities in the lymphatic network, but symptoms only become noticeable later in adulthood.
This delayed onset can make the condition more challenging to identify because swelling in older adults can also stem from issues such as venous insufficiency, obesity, heart disease, kidney problems, or infections. Therefore, diagnosis focuses heavily on distinguishing lymphedema from other causes of edema.
Initial Clinical Evaluation
Diagnosis begins with a thorough medical history and physical examination. This is often the most important stage because lymphedema tarda has particular patterns that an experienced clinician can recognize.
Medical History Review
A provider asks about:
- Age of symptom onset
- Progression of swelling (slow and chronic vs. sudden and painful)
- Family history of primary lymphedema
- Any prior surgeries, injuries, or infections
- Presence of risk factors for secondary lymphedema
- Lifestyle factors, such as level of activity or weight changes
Patients with lymphedema tarda typically report:
- Swelling beginning in one or both legs
- Gradual worsening over time
- Symptoms relieved temporarily by elevation but not fully resolved
- No clear triggering event
Physical Examination
The clinician examines the limbs for signs characteristic of lymphedema, such as:
- Persistent swelling that does not fully disappear overnight
- Thickened or firm skin
- Positive Stemmer’s sign (inability to pinch the skin at the base of the second toe or finger)
- Asymmetrical limb appearance
- Swelling involving the foot, which helps differentiate it from venous disease
Physical examination helps rule out common look-alike conditions and determines whether further testing is needed.
Ruling Out Other Causes of Swelling
Because many illnesses can cause leg swelling, diagnosing lymphedema tarda requires eliminating alternative explanations. Doctors may order:
Blood Tests
While bloodwork does not diagnose lymphedema directly, it helps exclude:
- Kidney disease
- Liver disease
- Thyroid dysfunction
- Heart failure
- Infection
Urinalysis and Basic Metabolic Panels
These help rule out systemic conditions that disrupt fluid balance.
Cardiac Evaluation
If swelling is suspected to be heart-related, clinicians may recommend:
- Electrocardiogram
- Echocardiogram
Venous Studies
Ultrasound Doppler studies check for:
- Venous insufficiency
- Deep vein thrombosis (DVT)
Since venous issues are a more common cause of swelling, ruling them out is critical before diagnosing lymphedema tarda.
Imaging Studies for Lymphatic System Assessment
Once other causes of swelling are excluded, imaging tests may be used to visualize how lymph fluid moves through the body. These tests confirm whether the lymphatic system is functioning normally.
Lymphoscintigraphy
This is the gold standard imaging test for diagnosing lymphedema.
How it works:
- A small amount of radioactive tracer is injected under the skin.
- A gamma camera tracks how the tracer moves through lymphatic vessels.
Findings in lymphedema tarda may include:
- Delayed or absent lymph transport
- Dermal backflow (fluid moving backward toward the skin)
- Missing or underdeveloped lymphatic channels
Lymphoscintigraphy is especially helpful for distinguishing primary from secondary lymphedema.
Indocyanine Green (ICG) Lymphography
This imaging test has become more popular in recent years because it provides real-time, high-resolution images of superficial lymphatic flow.
- A fluorescent dye is injected into the skin.
- A special infrared camera maps the lymphatic pathways.
ICG lymphography is often used not only for diagnosis but also for planning surgical treatments such as lymphovenous bypass.
MRI Lymphangiography
MRI can show:
- Lymphatic vessel structure
- Soft-tissue thickening
- Fluid accumulation
It is useful in complex cases or when surgical planning is required.
Ultrasound of Soft Tissue
While not specific for lymphedema, ultrasound helps identify:
- Thickened subcutaneous tissue
- Absence of fluid pockets that appear in venous disease
This makes ultrasound a supportive tool rather than a diagnostic one.
Staging Lymphedema Tarda After Diagnosis
Once lymphedema tarda is confirmed, clinicians determine the stage of the disease. Staging guides treatment decisions and helps track progression.
Common staging systems include:
International Society of Lymphology (ISL) Staging
- Stage 0: No visible swelling yet, but lymphatic damage is present.
- Stage I: Soft swelling that improves with elevation.
- Stage II: Permanent swelling, tissue thickening, and positive Stemmer’s sign.
- Stage III: Severe enlargement, skin changes, and significant fibrosis.
Most patients with lymphedema tarda present in Stage I or II because symptoms appear gradually in adulthood.
Developing a Personalized Treatment Plan
Accurate diagnosis is the key to effective treatment. Once identified, lymphedema tarda is typically managed using Complete Decongestive Therapy (CDT), which includes:
- Manual lymphatic drainage
- Compression therapy
- Exercise
- Skin care
In more advanced or resistant cases, surgical treatments such as lymphatic reconstruction or liposuction-based procedures may be considered. Imaging results play a major role in deciding whether surgery is appropriate.
Why Early Diagnosis Matters
Because lymphedema tarda progresses over time, early diagnosis leads to better outcomes. Delayed treatment can result in:
- Chronic skin thickening
- Increased risk of infections
- Greater limb enlargement
- Reduced mobility
- More complicated treatment needs
Conversely, early intervention can significantly slow or halt progression and improve quality of life.
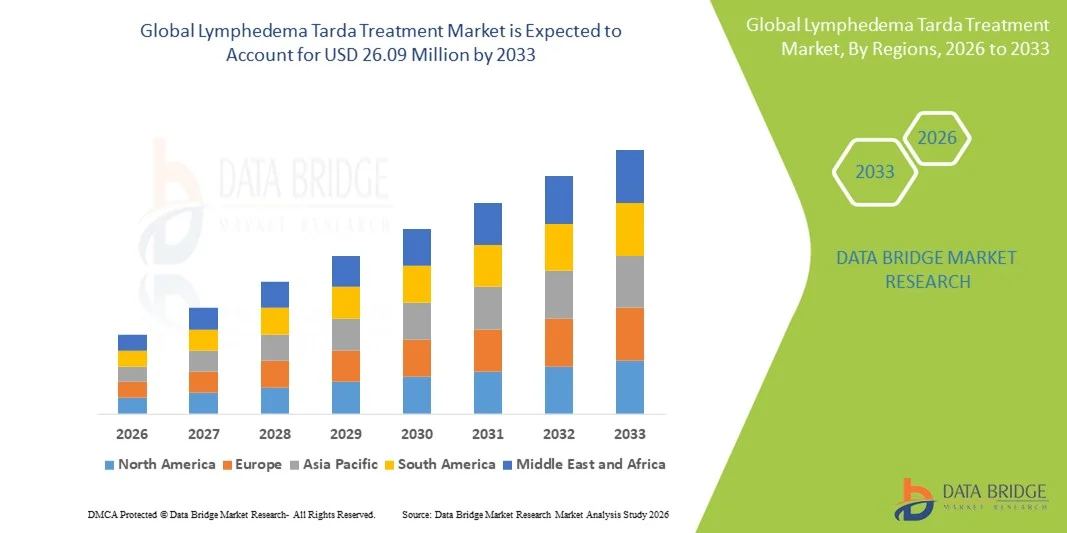
Growth Rate of Lymphedema Tarda Treatment Market
According to Data Bridge Market Research, the lymphedema tarda treatment market was estimated to be worth USD 13.53 million in 2025 and is projected to grow at a compound annual growth rate (CAGR) of 8.55% to reach USD 26.09 million by 2033.
Learn More: https://www.databridgemarketresearch.com/reports/global-lymphedema-tarda-treatment-market
Conclusion
Diagnosing lymphedema tarda is a step-by-step process that involves careful evaluation, ruling out other causes of swelling, and using specialized imaging to assess lymphatic function. Because symptoms emerge later in life and mimic other common conditions, a comprehensive diagnostic approach is essential. With accurate diagnosis, patients can begin personalized treatment to manage symptoms effectively and maintain long-term limb health.






0 Comments